Pressure ulcers (pressure sores)
Pressure ulcers (also known as pressure sores or bedsores) are injuries to the skin and underlying tissue, primarily caused by prolonged pressure on the skin.
They can happen to anyone, but usually affect people confined to bed or who sit in a chair or wheelchair for long periods of time.
Symptoms of pressure ulcers:
Pressure ulcers can affect any part of the body that’s put under pressure. They’re most common on bony parts of the body, such as the heels, elbows, hips, and base of the spine.
They often develop gradually, but can sometimes form in a few hours.
Early symptoms:
Early symptoms of a pressure ulcer include:
- part of the skin becoming discolored – people with pale skin tend to get red patches, while people with dark skin tend to get purple or blue patches
- discolored patches not turning white when pressed
- a patch of skin that feels warm, spongy, or hard
- pain or itchiness in the affected area
A doctor or nurse may call a pressure ulcer at this stage a category 1 pressure ulcer.
Later symptoms:
The skin may not be broken at first, but if the pressure ulcer gets worse, it can form:
- an open wound or blister – a category 2 pressure ulcer
- a deep wound that reaches the deeper layers of the skin – a category 3 pressure ulcer
- a very deep wound that may reach the muscle and bone – a category 4 pressure ulcer
When to get medical advice?
- If you’re at home or in a care home, tell your healthcare team as soon as possible if you develop symptoms of a pressure ulcer. It’ll probably continue to get worse if nothing is done about it.You should be regularly monitored and offered advice and treatment to reduce the risk of pressure ulcers, but sometimes they can develop even with the highest standards of care.If you’re recovering from illness or surgery at home, or you’re caring for someone confined to a bed or a wheelchair, if you think you or the person you’re caring for might have a pressure ulcer, ask for help immediately!
- Get medical advice immediately if there is:
- red, swollen skin
- pus coming from the pressure ulcer or wound
- cold skin and a fast heartbeat
- severe or worsening pain
- a high temperature
These symptoms could be a sign of a serious infection that needs to be treated as soon as possible.
Mkare can help!
If you are or if you caring for a person who is at high risk of developing a pressure sore, Mkare can help you. Not only with caring for pressure sores, but most importantly, helping you PREVENT pressure sores!
Who's most at risk of getting pressure ulcers?
- Anyone can get a pressure ulcer, but the following things can make them more likely to form:
- being over 70 – older people are more likely to have mobility problems and skin that’s more easily damaged through dehydration and other factors
- being confined to bed with illness or after surgery
- inability to move some or all of the body (paralysis)
- obesity
- urinary incontinence and bowel incontinence
- a poor diet
- medical conditions that affect blood supply, make skin more fragile or cause movement problems – such as diabetes, peripheral arterial disease, kidney failure, heart failure, multiple sclerosis (MS) and Parkinson’s disease
Preventing pressure ulcers
Pressure ulcers can be serious and lead to life-threatening complications, such as blood poisoning and gangrene. However, taking some simple steps can reduce the chance of pressure ulcers developing. Pressure ulcers are a key indicator of the quality and experience of care. That is why Mkare pays great attention to preventing rather than treating pressure ulcers. We believe that professional Risk assessments and Care planning can prevent a majority of pressure-caused ulcers.
Mkare Prevention strategies:
Surface
Equipment/support surfaces to relieve pressure and prevent skin damage should be used and evaluated regularly to review their effectiveness. Use a foam mattress or one that is filled with gel or air.
Skin inspection
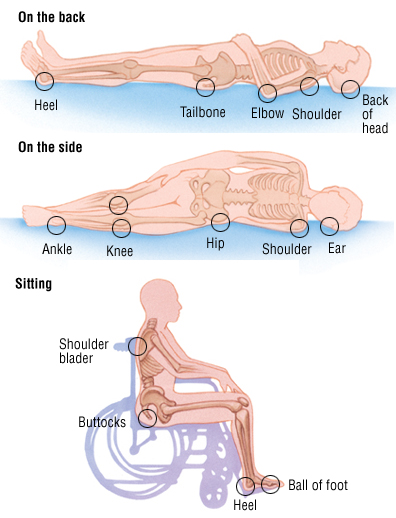
Body inspection has to be done every day from head to toe. Pay special attention to the areas where pressure ulcers often form. These areas are the:
- Heels and ankles
- Knees
- Hips
- Spine
- Tailbone area
- Elbows
- Shoulders and shoulder blades
- Back of the head
- Ears
Skincare
Treat the skin gently to help prevent pressure ulcers.
- When washing, use a soft sponge or cloth. DO NOT scrub hard.
- Use moisturizing cream and skin protectants on the skin every day.
- Clean and dry areas underneath breasts and in the groin.
- DO NOT use talc powder or strong soaps.
- After urinating or having a bowel movement area has to be cleaned right away and dried well
Keep moving
Repositioning and early mobilization are imperative in the prevention of bedsores. Patients who are identified as at risk of PU development need repositioning frequently. Where possible, patients should be encouraged to do this themselves.
Nutrition
Very important is to have a healthy, balanced diet that contains enough protein and a good variety of vitamins and minerals, as well as good hydration.